Large Language Models Take Center Stage: Potential for Critical Care Applications
INTRODUCTION
In 2022, the medical community was introduced to the capabilities of ChatGPT – a popular large language model (LLM) that performed exceptionally well in medical problem solving, scoring above 85% on both USMLE Step 1 and Step 2. ChatGPT is a chatbot composed of an advanced language model from the family of Generative Pretrained Transformer (GPT) models designed by OpenAI (San Francisco, California) in 2018. It is currently the largest publicly available LLM.1 ChatGPT was not specifically designed for a medical interface, yet it accomplished this task by instantaneously analyzing vast amounts of real-time data. It autonomously builds on previous functions, continuously improving its capabilities.2 LLMs are a subset of artificial intelligence (AI) designed to mimic human text and language processing abilities. LLMs utilize deep-learning algorithms, such as neural nets, to learn from text-based datasets. Vast amounts of datasets allow the LLM to analyze patterns and context of the text, learning statistical correlations between relative words and their position. This enables the LLM to predict which words are most likely to follow when presented in a given phrase.
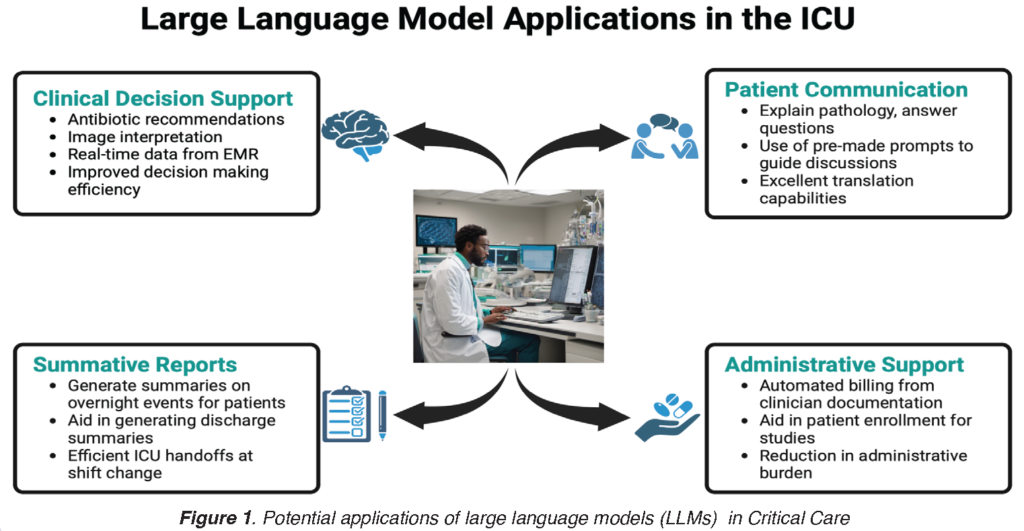
ChatGPT’s popularity and utility have increased exponentially in recent months, as it demonstrates value and efficiency across a wide variety of tasks. Numerous competitors have also entered the field, including Google’s Bard, Meta’s Llama, X’s (formerly Twitter) Grok, and Anthropic’s Claude to name a few. Also, many LLMs trained on healthcare data, including electronic healthcare record data, have been developed since then.3 The ushering in of LLMs for application in virtually every industry begs the question – how can we leverage LLMs in the intensive care unit (ICU) to improve patient outcomes and enhance the workflow of clinicians? (Figure 1)
OPPORTUNITIES
Clinical Decision Support
Within the ICU, chatbot-based LLMs can serve as an extension of the intensivist and a decision support tool for clinicians. In this context, LLMs would be most effectively utilized if they were developed “in house” for use in a specific hospital system with their electronic medical record (EMR). This would ensure compliance with standard operating procedures, chatbot recommendations tailored to community antibiograms, hospital pharmacy formularies, and real-time data pulled in from the EMR to aid in decision support. Imagine a scenario where a patient is admitted to the ICU in septic shock, and a LLM is able to make recommendations for pressors (while citing sources) based on bedside hemodynamic data, suggests initial antibiotics based on blood cultures or disease pathology, and is able to interpret initial radiographic imaging. In this hypothetical scenario, the added value in speed of decision-making and cognitive offloading to the intensivist presents a use case for LLMs in the ICU as they are further honed for the medical community.
Patient Communication
Conversations with patients and family members can often be challenging to navigate in the ICU. LLMs can help improve these communications with grace and compassion.4 Additionally, chatbot-based LLMs are highly valuable as a tool for patient communication to explain pathology and prognosis and answer patient questions on their own time. Patients and families can be given a QR code, email, or EMR message that generates a pre-determined prompt that can be copied into LLM-based chatbots. This prompt primes the AI model for its role and guides the conversation on the patient’s own level of understanding.5 Finally, LLM’s abilities to surpass language barriers offers tremendous value at the bedside. LLMs can be programmed to understand and respond in multiple languages with the click of a button, thereby providing an effective means of constant communication with patients who speak another language.
Summative Reports
One of the primary roles of LLMs in any setting is to sift through large amounts of available data and generate summary statements for the end user. The ICU presents a perfect environment to leverage this feature, as vast amounts of data are generated for each patient. LLMs can generate summative reports for patients on the unit overnight where notable events, abnormal lab results, imaging results, blood product transfusions, etc are pulled from the EMR and detailed in a concise report for sign-out to the day team. Such a use case would improve ICU efficiency and workflow organization with sign-outs at shift change. These capabilities can also be used for communications to generate discharge summaries in formats that are meaningful to the patients and their families.5
Administrative support
One of the promises LLMs hold in healthcare is their ability to help with documentation in the electronic health record (EHR). Clinician’s note documentation in EHR has been noted to be one of the key reasons for burnout. Relieving clinicians of this stress while caring for critically ill patients is likely to be immensely beneficial. Billing derived from clinician documentation and its automation is another potential use case where LLMs have the potential to reduce clinicians’ administrative burden.6 LLMs also hold the promise to support research by making the process of patient enrollment and measuring treatment effects easier.7 Lastly, for quality improvement, providing summarized insights of collected data in an efficient and effective manner is likely to improve the continuous improvement process in healthcare.
Education
With the infodemic in healthcare research and publications, LLMs can help provide curated information efficiently.8 LLMs can also help curate the information into formats such as presentations and documents, which are more effective. Assistance with curriculum design, filtering through trainee applications, and assistance with letters of recommendation are just some of the additional tasks LLMs are currently being evaluated for.9
CHALLENGES
Despite the potential benefits of LLMs in critical care medicine, there are significant challenges that must be addressed before widespread implementation can occur. One of the primary challenges is data privacy. Patient data are sensitive and must be protected from unauthorized access. Healthcare data are especially sensitive due to the risk of discrimination if wrongfully disclosed. The use of LLMs requires the collection and storage of large amounts of patient data, which further undermines public confidence in AI, given the general increase in the frequency of data breaches and inappropriate data use.10
Moreover, AI models face the notorious “black box” problem. Although these models can solve complex critical thinking problems, they are not always able to produce an explanation for a given response or solution.11 Additionally, a chatbot’s responses become tailored to the user as the algorithm refines responses based on user preferences. This can limit patients’ awareness of alternatives and gradually diminish their role in the patient-physician relationship.11 While users can train the chatbot simply by using it, the training data from which the chatbot structures its intelligence and responses can be inherently biased if it does not accurately represent the people it serves.12
These limitations can be mitigated by continuously training AI models with updated standards of medical care, incorporating medical knowledge explicitly within the training data, and promoting diversity in the field of AI.
CONCLUSIONS
LLMs have the potential to revolutionize healthcare by serving as an adjunct to the tools physicians use to improve patient care. The newer multimodal models, which can use various modalities of data, including text, variables, and images, to deliver multimodal responses, are likely to bring in even more enhanced capabilities in the near future.13 Within the field of critical care, LLM-based chatbots can aid in clinical decision support, help with goals of care discussions, and summarize the large data sets generated by patients in the ICU. Although measures must be in place to ensure the protection of patient data and minimize model bias, the integration of AI into the workflow of the ICU has the potential to improve patient outcomes and overall satisfaction with the delivery of care.
SOCCA Interchange Newsletter | Volume 35 | Issue 2 | Summer 2024 | Large Language Model Image
REFERENCES
- OpenAI. ChatGPT: Optimizing Language Models for Dialogue. 2022. https://openai.com/blog/chatgpt/
- Nori H, King N, McKinney SM, Carignan D, Horvitz E. Capabilities of GPT-4 on Medical Challenge Problems. 2023
- Peng, C., Yang, X., Chen, A. et al. A study of generative large language model for medical research and healthcare. npj Digit. Med. 6, 210 (2023). https://doi.org/10.1038/s41746-023-00958-w
- Ayers JW, Poliak A, Dredze M, et al. Comparing Physician and Artificial Intelligence Chatbot Responses to Patient Questions Posted to a Public Social Media Forum. JAMA Intern Med. 2023;183(6):589–596. doi:10.1001/jamainternmed.2023.1838
- Zaretsky J, Kim JM, Baskharoun S, et al. Generative Artificial Intelligence to Transform Inpatient Discharge Summaries to Patient-Friendly Language and Format. JAMA Netw Open. 2024;7(3):e240357. doi:10.1001/jamanetworkopen.2024.0357
- Cascella M, Semeraro F, Montomoli J, Bellini V, Piazza O, Bignami E. The Breakthrough of Large Language Models Release for Medical Applications: 1-Year Timeline and Perspectives. J Med Syst. 2024 Feb 17;48(1):22. doi: 10.1007/s10916-024-02045-3. PMID: 38366043; PMCID: PMC10873461.
- Jin Q, Wang Z, Floudas CS, Chen F, Gong C, Bracken-Clarke D, Xue E, Yang Y, Sun J, Lu Z. Matching Patients to Clinical Trials with Large Language Models. ArXiv [Preprint]. 2024 Apr 27:arXiv:2307.15051v4. PMID: 37576126; PMCID: PMC10418514.
- Awasthi, R., Mishra, S., Grasfield, R., Maslinski, J., Mahapatra, D., Cywinski, J. B., ... & Mathur, P. (2024). Artificial Intelligence in Healthcare: 2023 Year in Review. medRxiv, 2024-02.
- Abd-Alrazaq A, AlSaad R, Alhuwail D, Ahmed A, Healy PM, Latifi S, Aziz S, Damseh R, Alabed Alrazak S, Sheikh J. Large Language Models in Medical Education: Opportunities, Challenges, and Future Directions. JMIR Med Educ. 2023 Jun 1;9:e48291. doi: 10.2196/48291. PMID: 37261894; PMCID: PMC10273039.
- Seh AH, Zarour M, Alenezi M, et al. Healthcare Data Breaches: Insights and Implications. Healthcare (Basel). 2020;8(2):133. doi:10.3390/healthcare8020133
- Xu L, Sanders L, Li K, Chow JCL. Chatbot for Health Care and Oncology Applications Using Artificial Intelligence and Machine Learning: Systematic Review. JMIR cancer. 2021;7(4):e27850-e27850. doi:10.2196/27850
- Zou J, Schiebinger L. AI can be sexist and racist - it’s time to make it fair. Nature (London). 2018;559(7714):324-326. doi:10.1038/d41586-018-05707-8
- Tu, T., Azizi, S., Driess, D., Schaekermann, M., Amin, M., Chang, P. C., ... & Natarajan, V. (2024). Towards generalist biomedical ai. NEJM AI, 1(3), AIoa2300138.



































