Billing for Advance Care Planning: A Missed Opportunity?
Advance care planning (ACP) is a process that supports adults at any age or stage of health in understanding and sharing their values, goals, and preferences regarding future medical care 1. The goal of ACP is to help ensure that people receive medical care that is consistent with their preferences during serious and chronic illness 2. At the Cleveland Clinic, we operationally defined ACP as having two elements: documentation of the surrogate decision-maker in the electronic medical record (EMR) for all adult patients and goals of care discussion documentation for seriously ill patients. Ideally, this conversation between a seriously ill patient with a chronic condition and their primary provider would happen long before the moment of a critical illness crisis.
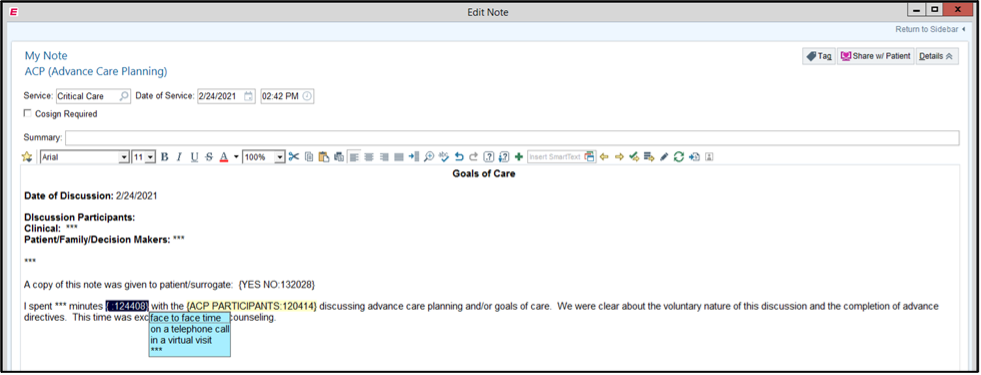
However, intensivists are often the first providers to have these conversations with patients or their loved ones. It can be challenging to establish an effective rapport and engage with patients or their loved ones during these emotionally charged discussions. It takes empathy, compassion, and an open mind on our parts to communicate clearly what patients or their loved ones can anticipate based on the decisions they make. The conversations are nuanced by the patient’s personal beliefs, culture, religion, language barriers, medical literacy, and previous interactions with the healthcare system. Our goals as intensivists should be to help patients and their loved ones make informed decisions that are congruent with their personal goals and priorities. The ACP discussion is often documented within the daily progress note. Alternatively, it is currently recommended that healthcare systems dedicate separate space within the EMR to document ACP as a “single source of truth” for easy access and shared understanding across providers. At the Cleveland Clinic, the End-of-Life Center in collaboration with the Information Technology department has pioneered an ACP navigator for Epic and created an ACP note type with a template for uniform documentation (Figures 1-3). This navigator is available to other systems to adopt.
Intensivists routinely have these discussions but may be unaware of associated opportunities for professional charge capture. ACP falls under “individual billing” by licensed independent providers per state law, such as that done by physicians, clinical nurse specialists, nurse practitioners, and physician assistants. Non-independent licensed providers have to be qualified and authorized to provide these services in the state that they practice. They are referred by the licensed independent provider, and they can bill under “team billing”.
Time spent on ACP conversations for critically ill patients should be counted toward critical care time within the interval billing framework. Critically ill patients deemed to have capacity should be engaged for an ACP discussion. For patients deemed to lack decision-making capacity, the provider will have their ACP conversations with the surrogate decision maker/s by state hierarchy. Time spent on these conversations aggregates towards the total critical care time on that calendar day. From a billing standpoint, critical care reflects the time required for directly managing the patient, composing the note, evaluating laboratory values, independently evaluating radiographic images, discussing the patient’s care with consultants, and—importantly—ACP conversations. Within a 24-hour day, the first 74 minutes of these activities are captured with a 99291 CPT code and any additional time equal to or greater than 75 minutes is captured with a 99292 code in blocks of 30 additional minutes.
ACP billing opportunities are often missed when the ACP discussion is conducted with patients (or their surrogates) who are not critically ill and would normally be assessed an evaluation and management (E&M) code (e.g., CPT 99232 for level 2 or 99233 for level 3). In this scenario, ACP discussions can be captured with additional CPT codes. Illustrating this, we present a case scenario from an ICU within a regional satellite hospital.
Case: A 76 year-old male with history of hypertension presented to his primary care provider with a one year history of weight loss. This prompted abdominal computed tomography, which demonstrated a pancreatic mass with lesions involving the liver, for which a biopsy was done. Three days later he presented to a free-standing Emergency Room with fever, malaise and dyspnea. He had a modestly elevated lactate of 4 and was requiring 2 liters of supplemental oxygen via a nasal cannula. The emergency room called the ICU with a diagnosis of community acquired pneumonia and requested ICU admission for closer monitoring. After reviewing the chart, it was noted the biopsy revealed metastatic pancreatic cancer. We admitted the patient, gently resuscitated him, and lactate and oxygen requirements resolved within a few hours. The patient was assessed a level 2 E&M code (i.e., CPT 99232). When the patient’s spouse arrived, we had a 20-minute ACP discussion with them. Given the gravity of his diagnosis, he did not want to receive cardiopulmonary resuscitation or to be intubated and mechanically ventilated.
In this scenario with a patient assessed an primary E&M code rather than a critical care code: CPT code 99497 can be used for 16 to 30 minutes of face-to-face ACP conversations and CPT code 99498 for subsequent 30 minute blocks. Table 1 details the average payments for the billing codes 3. During the COVID-19 pandemic, CMS published the Interim Final Rule allowing telehealth services to bill CPT 99497 and 99498 via virtual (audio and video) or audio only visits 4.
ACP discussions in the context of a critically ill patient should be ideally documented in a separate ACP note and accounted for in the aggregate critical care billing time. ACP discussions for patients assessed E&M codes should be documented separately in an ACP note and billed for according to the duration of the conversation by the separate time-based codes 99497 and 99498.
Table 1: Description of CPT Codes and national average payment 3
| CPT Code | Description | National Average Non-Facility Rate/Facility Rate |
|---|---|---|
| 99497 | Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate | $85.99/$79.54 |
| 99498 | Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure) | $74.88/$74.52 |
Figure 1: Advance Care Planning navigator in Epic
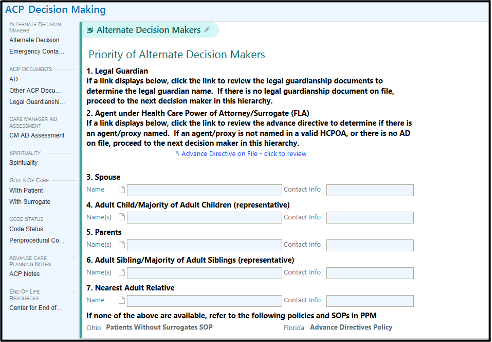
Figure 2: Advance Care Planning template
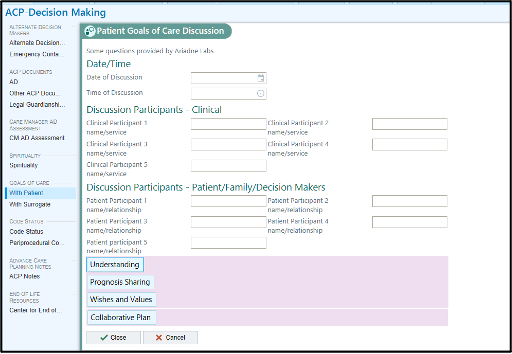
Figure 3: Advance Care Planning note template
References
- Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary delphi panel. J Pain Symptom Manage. 2017 May;53(5):821-832.e1.
- Sokol-Hessner L, Zambeaux A, Little K, et al. “Conversation ready”: a framework for improving end-of-life care, 2nd ed.. IHI White Paper. Boston, Massachusetts: Institute for Healthcare Improvement; 2019. Available online: ihi.org.
- Centers for Medicare and Medicaid. Medicare learning network fact sheet: advance care planning.. Pub Oct 2020, accessed March 15, 2021. Available online: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/MLN-Publications-Items/ICN909289.
- American College of Phsyicians. Summary: CMS interim final rule on CARES act. Pub March 2020, accessed March 15, 2021. Available online: https://www.acponline.org/system/files/documents/advocacy/where_we_stand/assets/summary-interim-final-rule-cares-act.pdf






































