COVID-19 Intubations: 10.7% Risk To Healthcare Workers?!
Subtitle: A summary of … El-Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. 2020 Nov;75(11):1437-1447
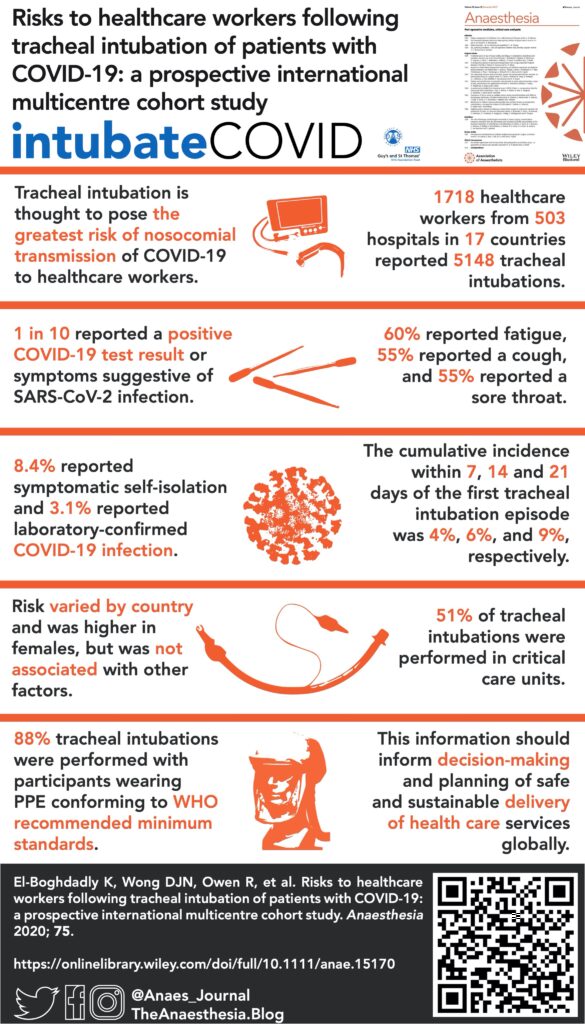
The risk to healthcare providers of intubating patients with COVID-19 is a global concern, but data are scarce despite the presumably high risks. Surprisingly, the results of a recent study published in Anaesthesia by El-Boghadadly et al. suggest that the risk of transmission, hospitalization, and/or self-quarantine may be slightly higher than 10% 1!
They present data from a prospective international multicenter cohort study based upon self-reported data in the new intubateCOVID registry. The registry includes data reported by 1,718 healthcare workers who reported 5148 intubations between March 23 and June 2, 2020. Roughly half of those intubations took place in the ICU. Of the participants, composed primarily of anesthesiologists followed by intensivists, 184 (10.7%) reported the primary composite endpoint: a positive COVID-19 test, hospitalization, or self-imposed quarantine for COVID-19-like symptoms. As the accompanying graphic shows, 3.1% of participants had a laboratory-confirmed positive test, and 2 required hospitalization. The cumulative incidence of positive endpoints increased over time.
Healthcare workers were greatly affected by the SARS-CoV-1 outbreak, representing 21% of infected patients. As we have learned how SARS-CoV-2 may behave differently, it is important to compare this current study to other available data, however limited. A recent study 2 found the incidence of a positive COVID-19 test was approximately 4% in front-line healthcare workers, compared to 0.33% for the general community. A study from Wuhan, China indicated that healthcare workers in high-risk departments, such as the ICU or the surgical department, had a higher risk of infection but was unable to quantify how much, if any, risk is attributable to airway management 3. In a survey study of 105 anesthesiologists and intensivists at a New York City hospital 4, 61 (58%) reported a workplace exposure (mostly related to airway management), 26% of those reported COVID-19-like symptoms after that exposure, but only 12% of providers tested were found to be positive for antibodies. That was the same incidence of positive antibody testing for those reporting no exposure, and the authors concluded the COVID-19 infections were most likely community acquired. (Interestingly, antibody-positive participants were twice as likely to use the subway). More recently, two new studies using optical particle sizers and lasers from the UK 5 and Australia 6 suggest that intubation does increase aerosolized particles. Interestingly, the UK study argues against labeling intubation an aerosolizing event as compared to a cough.
This study is timely as we navigate this new disease, and the authors should be commended for rapidly developing and deploying this prospective study and database. They investigate a question with very little data: what is the risk to healthcare workers when performing airway management? Strengths of this study include its large, international reach (503 hospitals in 17 countries), and data collection is ongoing. The database contains a sizable quantity and variety of data, including an assessment of personal protective equipment (PPE) compliance. The database had enough follow-up data for over 5,000 intubations, adding to the validity of the data. It will be interesting to see how the data changes over time, especially with COVID-19 cases again rising globally. Finally, the COVID-19 pandemic has been fraught with PPE shortages. Depending on how long you’ve been wearing your current N95 mask, you may either find it terrifying that 12% of these intubations were completed without WHO-recommended PPE or be relieved that 88% of them did conform to current guidelines. There was no association with reporting the primary outcome and the PPE combination used, but this may be due to the vast majority of registry participants (88%) wearing some combination of the recommended protective gear. As the pandemic continues (or worsens), and PPE shortages potentially re-manifest, risks to healthcare workers who do not have recommended protective gear may become better known.
Weaknesses include self-reporting as the sole means of data collection, an unclear assessment of temporal associations between exposure and outcomes, and little assessment to external exposures. Reporting and sampling bias are certainly a concern. It is feasible that the self-reported data may overestimate the data – some of those who self-isolated but were not tested could have been negative. The authors discuss, however, the lack of widespread availability of asymptomatic testing means that it is possible the true transmission rate was actually underestimated. A wide range of incubation times have been reported for COVID-19 with a recent meta-analysis suggesting a mean of 6 days 7, and the authors here gathered data at 7, 14, and 21 days. The authors are clear that this study is unable to provide causality between intubation and symptoms, and it is possible the longer time intervals studied only permitted more external exposures and confounding.
An interesting follow-up study might be examining how to optimize testing for intubators. Only 54 providers had lab data confirming COVID-19 while 144 providers self-isolated for symptoms only. Both groups were removed from the workforce with significant impact to care teams and families. Might the varied symptoms and the hypervigilance of our providers lead to more self-isolation and resultant cost than is necessary? Could different provider testing schemes decrease the number of isolation days? As we face the colder months and a surge in cases, it is vital that we have some data to help us protect our staff and ensure the consistent availability of critical healthcare workers.
References
- El-Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. 2020; 75(11):1437-1447.
- Nguyen LH, Drew DA, Graham MS, et al. for the COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020; 5(9):e475-e483.
- Ran L, Chen X, Wang Y, et al. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020; Epub ahead of print.
- Morcuende M, Guglielminotti J, Landau R. Anesthesiologists' and intensive care providers' exposure to COVID-19 infection in a New York City academic center: a prospective cohort study assessing symptoms and COVID-19 antibody testing. Anesth Analg. 2020; 131(3):669-676.
- Brown J, Gregson FKA, Shrimpton A, et al. A quantitative evaluation of aerosol generation during tracheal intubation and extubation. Anaesthesia. 2020; Epub ahead of print.
- Dhillon RS, Rowin WA, Humphries RS, et al. for the Clinical Aerosolisation Study Group. Aerosolisation during tracheal intubation and extubation in an operating theatre setting. Anaesthesia. 2020; Epub ahead of print.
- McAloon C, Collins Á, Hunt K, et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open. 2020; 10(8):e039652.





































