Goals of Care Conversation in the Intensive Care Unit During the COVID-19 Pandemic
With the holiday season upon us, in the US and globally, ICUs (Intensive Care Units) are still struggling with the deadly COVID-19 pandemic. For the first time in our history, hospital systems are forced to scramble to allocate scarce resources such as nursing, respiratory therapists, ICU beds, oxygenation, and drug treatments that lack adequate amount of literature support. According to provisional data, in 2020, there were notable changes in the number and ranking of deaths compared with 2019. COVID-19 was the third leading cause of death in 2020, with an estimated 345 323 deaths, and was responsible for the substantial increase in total deaths from 2019 to 2020 [Table 1].
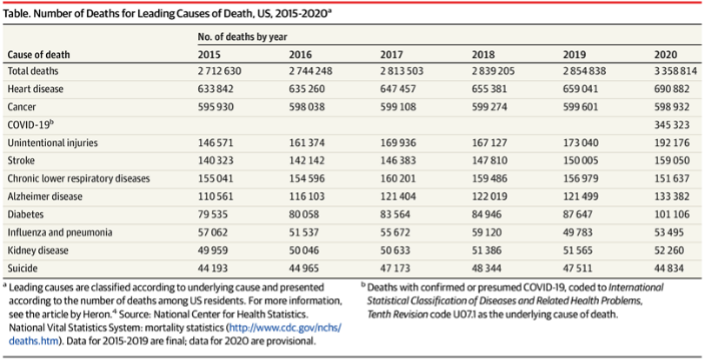
Table 1: Number of Deaths for Leading Causes of Death, US, 2015-2020
https://jamanetwork.com/journals/jama/fullarticle/2778234
There is also chaos amongst the public. During the past few months, we have experienced the divide amongst those who believe in the vaccine and those who do not. Since we live in the virtual internet era, medical information is easily accessed by the public, however this also comes with false information that the public may not be able to discern. Patients are requesting medications such as Ivermectin that have not been supported scientifically. This resulted in family members of patients versus the hospitals and their doctors standing in front of the judicial systems and are finally forced to administer treatments that are not backed by science. We learn that even clinicians are divided into what are believed to be the best treatment. This had left the public with confusion, doubt, and questioning the legitimacy of treatment enforced by our governing bodies from the FDA (Food and Drug Administration) and CDC (Centers for Disease Control). For example, there have been different recommendations and endorsement between the FDA and CDC.
Combine this chaos with the already over-worked, exhausted ICU providers, and with families who are experiencing the unexpected dying of their family member from COVID-19 and are restricted in their visitation rights—some of whom are demanding treatments that you believe have not been backed by science and could potentially cause more harm than benefit. This created a state of animosity and lack of trust between family members and their ICU providers. The lack of trust becomes apparent, especially for the particularly important goals of care conversation that need to take place between providers and family members. At times, this leads to suffering of the patient.
In the event we encounter a hostile interaction, we can refer to COVID Ready Communication Playbook | VitalTalk. This resource provides strategies on how to communicate and preference of what to say when emotions are high during an interaction with patients or their family members. The following is an example taken from VitalTalk on how to respond and the phrases we can use to diffuse these emotions:
| You people are incompetent! | I can see why you are not happy with things. I am willing to do what is in my power to improve things for you. What could I do that would help? |
| I want to talk to your boss. | I can see you are frustrated. I will ask my boss to come by as soon as they can. Please realize that they are juggling many things right now. |
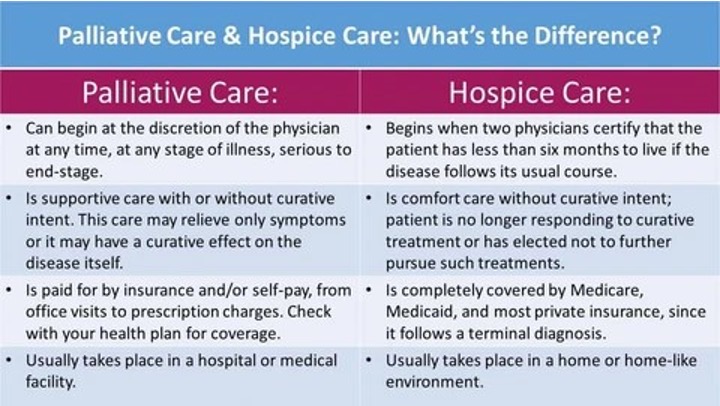
Regarding goals of care discussions, palliative care can enhance both the quality of end of life, as well as extend longevity of end of life. Goals of care conversations are essential to ensure high quality care for our critically ill patients. However, not all hospitals have palliative team consultants available all hours of the day, 24/7. Amidst the above barriers, the lack of trust from patients and their families, and time constraints during the pandemic in an overloaded ICU, are requiring more than ever a system or framework that helps with goals of care conversations in a pandemic. As the COVID-19 crisis continues, ICU clinicians face an urgent need to conduct goals-of-care conversations. To ensure an effective goals of care conversation, when possible, clinicians should initiate goals-of-care conversations ideally, among all patients admitted to the ICU, and especially the very sick. However, many ICU clinicians lack not only in time required to hold these conversations, but also lack the experience and training, so that they face deep uncertainty in planning, conducting, and evaluating such interactions. [Petriceks]. According to provisional data, in 2020, there were notable changes in the number and ranking of deaths compared with 2019. COVID-19 was the third leading cause of death in 2020, with an estimated 345 323 deaths, and was responsible for the substantial increase in total deaths from 2019 to 2020.
To help guide clinicians with a comprehensive and effective goals of care conversation, using a checklist or framework will help to adhere to best practices and cover key points for an effective goals-of-care conversation [7]. There are several frameworks that can help guide the clinicians such as REMAP, SUPER, or “Just Ask” conversation guide.
In this article, we will describe The GOOD and REMAP Framework, and the Three Stage Protocol. No matter which framework or checklist to use, they all provide person-centered, high-quality care that leads to positive satisfaction and outcomes for your patients, their families, and your organization [7].
The GOOD Framework
The GOOD framework was developed at the Stanford University School of Medicine and helps clarify uncertainties in working with older patients or those with serious illness particularly, though not exclusively, during the current pandemic. The framework, which stands for Goal, Option, Opinion, and Documentation, provides clinicians and their elderly patients in serious illness with steps and the resources to help with a successful goals of care conversation; it helps clinicians with the components to plan, conduct, and evaluate goals of care conversations. GOOD was developed for both palliative care clinicians and those nonpalliative care providers for use during the pandemic and ongoing [Petriceks].
The two primary purposes of the GOOD Framework (illustration 1) are:
- Concise mnemonic that is useful at any time beyond the pandemic
- Prepare the clinicians with resources and provide guidance of goals of care conversation to nonpalliative care clinicians, including resources in communicative strategies and empathic language. See Table 2 for empathetic responses.
Illustration 1
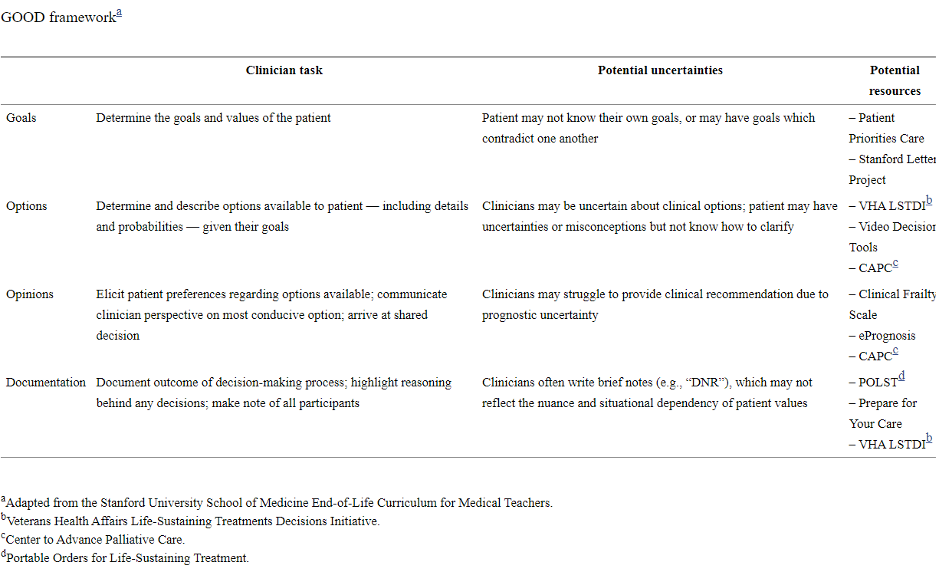
Table 2. Empathetic Responses
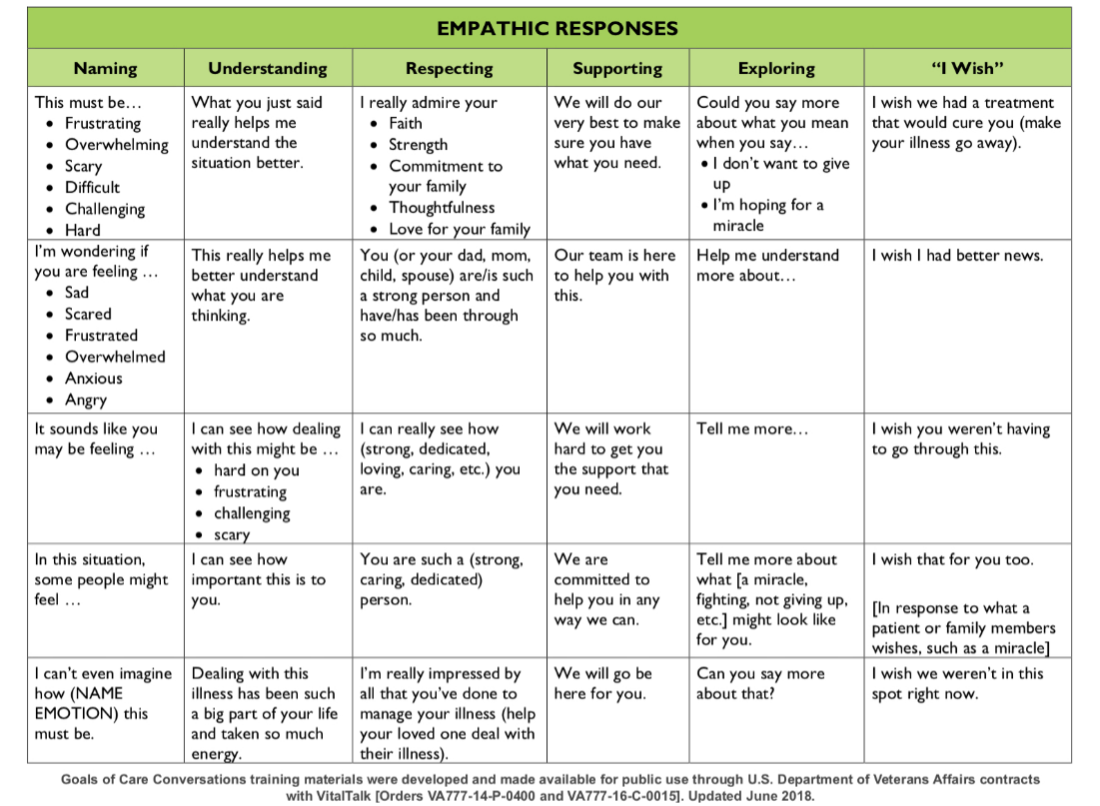
Graphic from Skillset Review - COVID-19 Curriculum (covidstudentresponse.org)
REMAP Framework
REMAP (Reframe, Expect, Map, Align, Plan) was published by the Journal of Oncology Practice in 2017. It provides a stepwise approach for complex goals of care conversations. It was originally developed to help oncologists who believed they had lack of training having goals of care conversations and that these conversations were occurring “too late” in cancer patients who were already diagnosed with advanced disease. This framework had been optimized for those late goals of care conversation where a clinical decision is needed urgently. It has been a commonly used framework that guides the clinicians to cover key components of the conversation [8]. With REMAP, the clinician can determine a patient’s primary values, goals, and fears, which will then help the clinician to develop a plan that honors those values, goals, and fears [table 3]. The processes underlying REMAP encourage oncologists and other clinicians to seek to understand and remain flexible, adapting their recommendations to what they hear from the patient, with ongoing revision based on the shared decision-making process. This will lead to patient-centered decisions that promote better end-of-life care [8].
Table 3: REMAP Framework
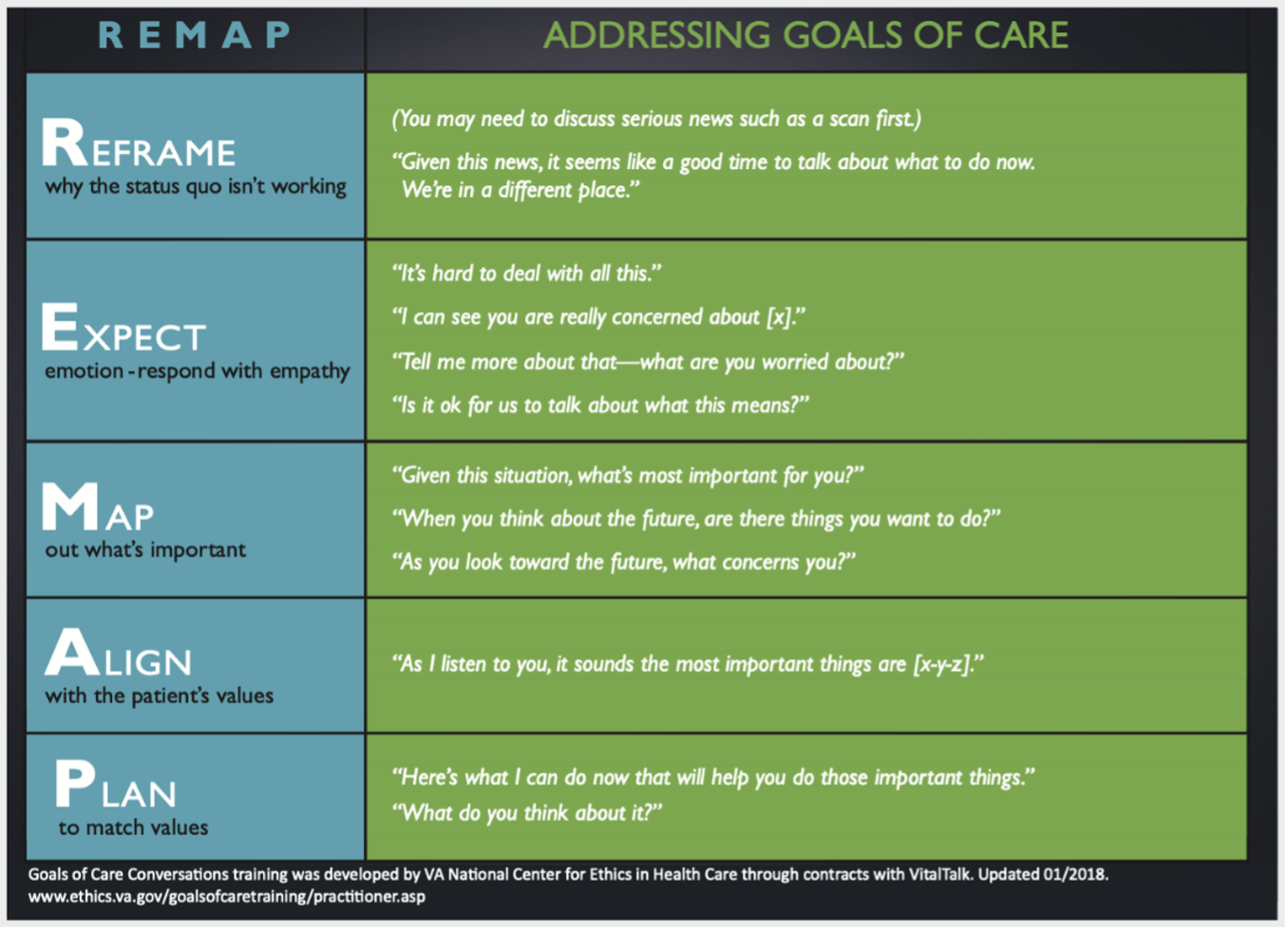
Graphic from Skillset Review - COVID-19 Curriculum (covidstudentresponse.org)
The Three-Staged Protocol
This protocol was developed to guide an ED-based COVID-19 palliative care response team, focused on providing high quality GOC conversations in time-critical situations [10]. Stage 1 is for sharing knowledge and prognosis. This stage can be somewhat challenging as COVID-19 medical management and treatments are rapidly evolving. The author recommends emphasizing functional status outcomes rather than focusing only on mortality or survival data. The clinicians should expect a strong emotional reaction from this news which needs time and support prior to initiating stage 2. In stage 2, the conversation involves discussion about goals of care. This can be obtained from determining the patient’s most important values and what makes them enjoy life. Finally, stage 3, the clinician emphasizes treatment options and makes recommendations that are in line with the patient’s most important goals and values.
Summary and Future Goals
COVID-19 pandemic can lead to rapid progression to respiratory failure necessitating mechanical ventilation. Currently, the mortality for those on mechanical ventilation is high, especially for the elderly and those with comorbidities such as diabetes mellitus and hypertension. In those who survived, the threat is of being on prolonged mechanical ventilation and inevitably bed-bound and cachectic for an undetermined time period. This had caused the intensivists and clinicians from all specialties other than palliative care to learn and provide goals of care conversation in an urgent manner, regardless of their previous training and experience in holding these conversations. Ideally, goals of care conversation should start early on all patients admitted to the ICU, and not only undertaken for those close to end of life. These conversations require more than one sitting and should be considered a process. Expect that the first conversation will not usually reveal a change in any medical plan management or goals of care. With news of poor prognosis, patients and their families need to be provided with sufficient time to process and grief, it is not a time to discuss goals of care at the same time. Future studies are needed in the development of goals of care conversation specifically for nonpalliative care ICU providers during a pandemic. In the meantime, the ICU clinicians can use and follow guidance from the GOOD and REMAP frameworks or the Three-Staged protocol as they help with a comprehensive approach in determining the patient’s most important values about their medical care and ultimately their satisfaction. It would be beneficial to have palliative care and goals of care conversation integrated into training programs or as requirement continuing medical education for those providers in intensive care.
Illustration 2
Where to obtain further resources and information:
- https://www.vitaltalk.org. For practical advice on how to talk about many difficult topics related to covid-19, including specific phrasing for patient and family conversations, read COVID Ready Communication Playbook | VitalTalk Quality Guidelines, Standards, & Measures | AAHPM
- Patient and Survivor Care | ASCO
- Center to Advance Palliative Care (2020) CAPC COVID-19 Response Resources. Retrieved from: https://www.capc.org/toolkits/covid-19-response-resources/ (18 April 2020). [Ref list]
Image taken from https://thedeathdeck.com/blogs/death-and-life/whats-the-difference-between-palliative-care-and-hospice
__________
References
- What the FDA wants doctors to tell patients asking for ivermectin | American Medical Association (ama-assn.org)
- https://jamanetwork.com/journals/jama/fullarticle/2778234
- https://www.nia.nih.gov/health/topics/palliative-care
- Source: VitalTalk 2019. https://www.vitaltalk.org
- Center to Advance Palliative Care (2020) CAPC COVID-19 Response Resources. Retrieved from: https://www.capc.org/toolkits/covid-19-response-resources/ (18 April 2020). [Ref list]
- Skillset Review - COVID-19 Curriculum (covidstudentresponse.org)
- Goals-of-Care Conversations: 3 Ways to Improve Your Skills - (acpdecisions.org)
- REMAP: A Framework for Goals of Care Conversations. Julie W Childers et al. J Oncol Pract. 2017 Oct.
- Goals of care and covid-19: A GOOD framework for dealing with uncertaintyAldis H. Petriceks, B.A.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7322160/
- Time-Critical Goals of Care in the Emergency Department during COVID-19: A Three-Stage Protocol Shunichi Nakagawa,MD. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7323252/pdf/JGS-9999-na.pdf





































