Results and Trends in the Anesthesia Critical Care Medicine Fellowship Match
Introduction
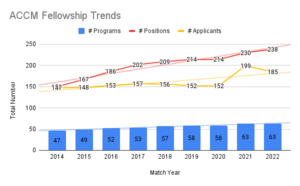
Anesthesia Critical Care Medicine (ACCM) is the oldest ACGME board-certified subspecialty within Anesthesiology and has seen tremendous growth over the past decade. In an effort to organize, streamline, and create a fair and equal process for fellowship recruitment, ACCM fellowship programs have participated in the SFMatch process since 2014. Over the past nine years we have increased the number of fellowship programs offering positions in the match by 35% and increased the number of positions by 58%. Despite the expansion at the programmatic level, the interest in the field has yet to catch up to the need, and we remain with unfilled positions throughout the country.
Results of the Match
After seeing a slight uptick in the 2021 cohort that was attributed to increased interest due to involvement in critical care rotations and the visibility of anesthesia-intensivist leadership revealed through the COVID-19 pandemic, we witnessed slight decreases in applicant registrations, the number of applicants that submitted a rank list, and the total number of matched applicants. While many were hopeful that the sharp increase in applications in 2021 would be a continuing trend, it instead may be an outlier, and the interest in the field of ACCM has a slower rate of rise than previously anticipated. The silver lining is that the interest is rising and we recruited a strong cohort of future intensivists across the country.
Highlights of the Match
The 2022 match process was smooth and collegial despite 29 programs remaining unfilled on Match Day. The match process is designed to be resident-centric, allowing resident preferences to drive the process, and 90% of applicants matched with their first-choice program. SOCCA has sponsored a match-exception agreement process for special circumstances such as residents matching to their home fellowship program and applicants committing to a two-year training agreement (full details regarding the policy around match exceptions can be found on the SOCCA website https://socca.org/fellowships-overview/). Up to 58% of the applicants used the match-exception agreement process to secure their positions. The most common reason (42% of applicants) for using this process was for the two year-training programs. Those pursuing two-years of consecutive training in ACCM followed by Adult Cardiothoracic Anesthesia (ACTA) represented 20% of the entire applicant pool and 35% of those solidifying their positions through the match exception process. Emergency Medicine (EM) residents are required to complete two years of training and therefore utilize the match exception process as well. EM applicants make up approximately 17% of the applicant pool and accounted for 30% of those utilizing the match exception process.
Trends in ACCM Compared to other Subspecialty Programs
Interest in Anesthesiology Fellowship Training Programs
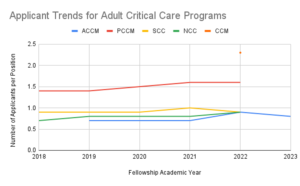
A common theme at the subspecialty update session at the annual Association of Anesthesiology Subspecialty Program Directors (AASPD) is the applicant to position ratio for individual subspecialties. While all fellowship programs have increased their offered positions over the past year, only ACTA and Pain Medicine continue to have more applicants than positions offered. ACTA, ACCM, and Pediatrics all had a slight decrease in applicants in 2022 (data for Regional and Acute Pain Medicine and Obstetric Anesthesia are not publicly available). Combining the number of fellowship positions available across the board, as seen in Figure 2, shows that the total number of positions approaches the total number of graduating residents in Anesthesiology training programs in the United States. This does not take into account non-ACGME accredited fellowships that are also increasing in number. Without an increase in the applicant pool, anesthesiology fellowship programs will continue to go unfilled across the majority of subspecialty programs.
Interest in Critical Care Medicine Across Specialties
Even prior to the COVID-19 pandemic, discussion of intensivist shortages throughout the nation loomed over our specialty. As a contributor to the workforce for critical care medicine, we join our colleagues in Pulmonary Critical Care Medicine (PCCM), Critical Care Medicine (CCM), Neurocritical Care (NCC), and Surgical Critical Care (SCC) to fulfill the need to train adult critical care physicians to address the public health shortage. All programs saw an increase in applicants during the first recruitment cycle after the pandemic. However, only NCC (34% increase from previous year) and PCCM (15% increase from previous year) reported a continuous uptick in applicants. PCCM and CCM remain the only programs to have more applicants than positions offered which is demonstrated in Figure 3. In order to increase intensivist coverage across our nation, our multidisciplinary specialty will need to support expansion in PCCM and CCM medicine positions to accommodate the increased demand in those specialties and/or develop ways to attract applicants into the surgical, anesthesia, and neurocritical care training programs.
Using Trends to Enhance Recruitment Strategies and Interest in ACCM
As mentioned above, attracting more applicants into our training programs is a goal of the current SOCCA Program Director’s Advisory Committee (PDAC). Analyzing the current trends in applications, highlighting unique pathways, and focusing on innovative curriculum are ways in which our committee will be leaning into these efforts.
Two-Year Fellowship Tracks
The most common match exception used amongst programs and applicants is for those pursuing ACCM and ACTA fellowships in a consecutive structure. This allows the applicant to focus on programs that can offer both positions, minimize moving twice, and allow longitudinal growth at the same institution. A joint task force between SOCCA PDAC and the Society of Cardiothoracic Anesthesia (SCA) is actively improving the application process and joint efforts for program innovation and structure. The PDAC also recognizes that critical care medicine is not limited to a combination with ACTA but also lends itself to those interested in maternal health and obstetrical anesthesia, regional and acute pain management, perioperative medicine, trauma anesthesia, and research. Designing innovative two-year programs can attract candidates that are developing specific academic or scholarly interests and improve interest in our specialty.
American Board of Anesthesia Sponsored Emergency Medicine Pathway
Emergency medicine physicians are able to train in critical care medicine through multiple pathways, including a formalized two-year training program associated with ACCM ACGME approved programs. In 2013, the American Board of Anesthesiology created a pathway for training programs to develop a second year of training to fulfill board certification requirements for EM trainees. We now have over 32 of the 63 registered ACCM fellowship programs approved with more programs working on their applications. Advertising our training program as a good fit for EM physicians is another way to increase our applicant pool for our fellowship training programs.
Obstetrical-Gynecology Trainees
Obstetrical and Gynecology (OBGyn) residents have shown an increased interest in critical care subspecialty training. With the current rates of maternal mortality in the United States and a global need to improve maternal health nationwide, providing an avenue for OBGyn physicians to train and become board certified in critical care medicine can help this mission. While the current interest is small, we have seen a slow increase in interest over the past three years in cross-specialty applicants. ACCM is a program well-fitted for OBGyn residents given our cross-specialty nature and collaborations within our obstetrical anesthesia divisions.
Critical Care Ultrasound Training and Certification Options
The National Board of Echocardiography (NBE) now offers a certification exam in Critical Care Echocardiography. ACCM programs have been leaders in Critical Care Ultrasound Training and continue to lead the way. Improving resources for programs to adequately train fellows in this area can attract candidates to the fellowship program. The NBE offers both a training pathway and a practice pathway for certification and both require fellowship training and/or critical care practice and billing time to acquire certification.
Return to Fellowship for Practicing Physicians for Community Needs
Given the overall need for a larger applicant pool beyond current trainees, creating avenues and limiting barriers for practicing physicians interested in the specialty to return to training is another way in which the PDAC is hoping to recruit into our programs. The COVID-19 pandemic put a lot of stress on community ICUs and many community anesthesiologists stepped up to staff and cover critical care units. We have seen physicians return to fellowship training with the goal of going back to their community hospitals to provide more formalized services to the ICU. Creating a space for private practice physicians to become involved in SOCCA and learn more about opportunities is another way to increase exposure to the benefits of formal fellowship training.
Integrated Critical Care Residency-Fellowship Training
In the last copy of SOCCA Interchange, the group at OHSU shared their positive experience with an integrated critical care training program. In this program, medical students match with the program directly and are set up to spend a total of five years at the same institution in which the critical care fellowship rotations are spread out over the last 24 months. Integrated programs like these are a way to recruit early and mentor residents for success in our specialty.
Call to Action for SOCCA Members
Consider these top five ways to help expand our applicant pool and recruit trainees into our amazing, rewarding, and innovative subspecialty.
1. Mentor a student - Start recruiting earlier!
2. Recommend and sponsor a resident - We need 20% of the current class to apply to ACCM!
3. Retweet the Program Spotlights during Recruitment Season: Follow SOCCA on Twitter and help us spread the word!
4. Highlight open fellowship positions when discussing anesthesia job searches: Send current CA3 residents to our website listing of programs or to the SFMatch listing (https://sfmatch.org/vacancies) of open 2023 fellowship positions when discussing their job search.
5. Collaborate with interdivisional and multidisciplinary colleagues: Discuss opportunities to provide dual-training programs within your department or support an emergency medicine or OBGyn resident to pursue ACCM as their preferred training pathway for critical care medicine.
*All data extracted from publicly available sources from SFMatch, NRMP, and AAMC. RAPM fellowship numbers extracted from asra.org.