Teaching Our Residents POCUS
Point-of-care ultrasound (POCUS) has become an integral part of the anesthesiologist and intensivist toolbox for the diagnosis and management of various disease states especially as ultrasound systems become more ubiquitous in our hospitals and increase in portability and ease of use1. This has been emphasized by the ABA in adding the application and interpretation of POCUS cardiac, lung, and abdominal imaging to the Applied Exam2. Working with residents and fellows, I often wonder about the most efficient and effective way to teach these skills in a busy clinical setting. How do we best integrate this into the trainee curriculum? How many exams are necessary for a trainee to become competent (independent)? Should residents strive for some sort of certification?
At the Medical College of Wisconsin (MCW), we have implemented a longitudinal curriculum starting from the resident’s PGY 1 year and continuing into the resident’s CA 3 year. This has integrated well within our existing simulation education. Given that each trainee has a different background and experience coming from medical school, we start with the basics. As an introduction, our PGY1 residents receive a didactic session followed by a hands-on course where we focus on cardiac and lung imaging on a standardized patient. Groups are small and limited to five residents per faculty member to allow sufficient personal instruction. Our CA 1 curriculum gives our residents exposure through our trauma simulation workshop where they practice and implement the EFAST exam, which is used routinely in our trauma bay. During the CA 2 and CA 3 years our residents receive a five-part curriculum. We increased this from 3 last year as a response to our residents' feedback. The curriculum goes through ultrasound basics/knobology, cardiac, lung, and abdominal imaging. Each session has a didactic portion followed by practical hands-on experience, keeping with small groups to allow sufficient instruction. These sessions have been rated as “extremely effective” by more than 80% of our residents. On our pre and post-test given to the residents before and after our POCUS course, self-reported knowledge scores increased from a mean of 4.67 SD 2.11 (out of 10) to 6.88 SD 1.86 (Table 1). The residents continue to practice their ultrasound skills as the opportunities arise either in the operating rooms or in our intensive care units.
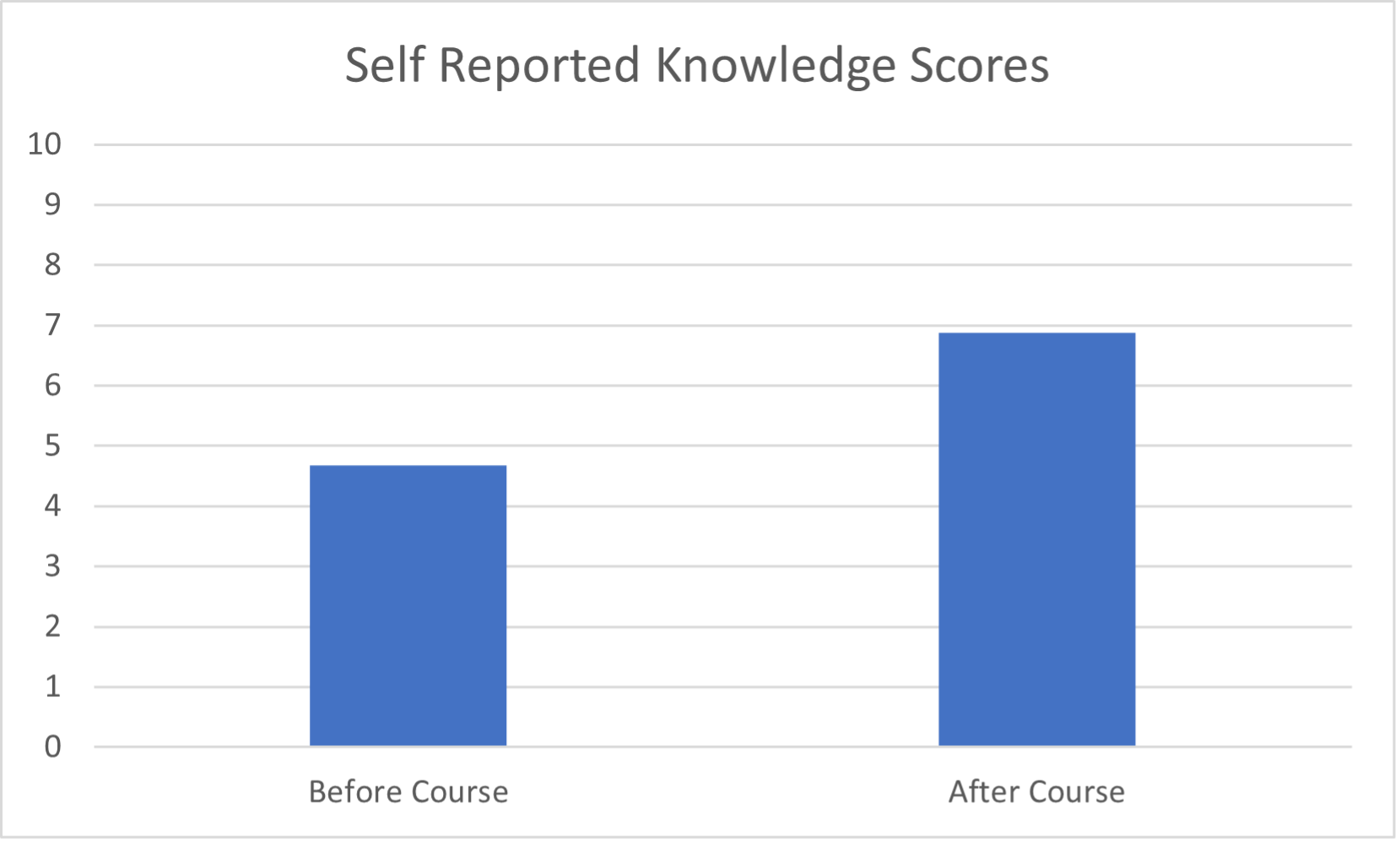
Table 1. Self-reported knowledge scores before and after our POCUS course (out of 10).
Our CA3’s can choose to take a two-week long POCUS elective. They focus on imaging patients in our PACU and our CVICU, with the ICU providing great exposure to various pathologies. A faculty member is available daily to review exams with each trainee. Each exam is saved into our PACS system allowing for quality review, not to mention a log of each exam the resident has completed. It is here that our residents can practice more advanced techniques such as calculating cardiac output, measuring valve gradients, estimating severity of valvular lesions and quantification of ventricular function. This elective course has received a lot of positive feedback and has quickly become one of our most popular electives.
Regarding competency, Clunie et al recently published that their residents needed 36 exams to reach an entrustment score of greater than 4 (may use independently) for cardiac exams and 8 for lung exams3. However, not each trainee learns at the same rate and there should be a system to evaluate resident competence prior to them being “signed off” to perform and interpret exams independently. Certification can be obtained through The American Society of Anesthesiologists Diagnostic POCUS Certificate Program. This is a structured online program which requires 100 cardiac, 20 lung, 20 gastric, and 20 fast exams as part of their certification process and requires mentor attestation. A motivated resident can certainly meet those numbers and obtain the certificate during the tenure of their residency with proper opportunities and mentorship. Certification can also be useful for hospital privileges in the future and maintenance of quality of POCUS examinations.
POCUS continues to gain popularity into our daily practice in the operating rooms and the ICU. At MCW we have integrated our POCUS curriculum within our existing simulation curriculum with encouraging results and good feedback from residents. Competency and certification are both goals that our residents can reasonably achieve.
- Naji A, Chappidi M, Ahmed A, Monga A, Sanders J. Perioperative Point-of-Care Ultrasound Use by Anesthesiologists. Cureus. 2021 May 24;13(5):e15217.
- The American Board of Anesthesiology. (2022, February). APPLIED Exam Objective Structured Clinical Examination (OSCE) Content Outline. Retrieved February 1, 2023, from https://www.theaba.org/wp-content/uploads/pdfs/OSCE_Content_Outline.pdf
- Clunie, M., O’Brien, J., Olszynski, P. et al.Competence of anesthesiology residents following a longitudinal point-of-care ultrasound curriculum. Can J Anesth/J Can Anesth 69, 460–471 (2022).





































