Updates from the Physiologically Difficult Airway Task Force: Delphi Consensus Summary
In October of 2020, SOCCA formed a task force to champion the cause of physiologically difficult airway (PDA) management. As is familiar to critical care anesthesiologists, in the contemporary era of airway management the physiologic challenges posed by patients requiring tracheal intubation outside of the operating room with, for example, right ventricular failure, cardiovascular instability, or severe hypoxemia, often surpass the technical challenges associated with intubation itself. This clinical gestalt has been increasingly supported over time by large-scale observational studies, including INTUBE and INTUPROS. As an organization composed of experts in applied complex cardiopulmonary physiology, SOCCA and its membership were well-positioned to make substantive contributions.
A critical mass of literature has amassed over time such that we now have practical, evidenced-based strategies to help inform PDA management in certain aspects, such as optimizing pre-oxygenation. However, the literature remains lacking in many other critically important aspects. Along those lines, SOCCA’s PDA Task Force identified an opportunity to develop expert consensus informed by a robust Delphi methodology to fill in these gaps, better inform practice, and identify areas for future research.
The PDA Task Force first conducted a literature review to identify clinical domains relevant to PDA management: definition/risk factors, team preparation and human factors, patient preparation and optimization, performing the procedure, and post-intubation care. Within these domains, Task Force members identified topics and questions key to clinical management, for which many have absent or limited evidence to inform best practice. The Task Force chartered a steering committee for the consensus effort, recruited an international expert panel, developed a survey tool, and then over seven Delphi rounds in 2023 identified areas of expert consensus and dissensus regarding PDA management.
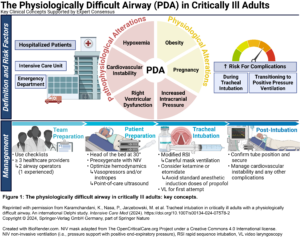
The results of this effort were recently published in Intensive Care Medicine. A key point that emerged was an expert consensus definition of a PDA: one in which the patient’s physiological and pathophysiological alterations increase the risk for complications during tracheal intubation and the transition to positive pressure ventilation. Hypoxemia, cardiovascular instability, right ventricular dysfunction, and increased intracranial pressure were felt to represent relevant pathophysiological alterations, whereas obesity and pregnancy were felt to represent relevant physiological alterations.
Key points for emphasis in different facets of clinical management are summarized below.
|
Team preparation and human factors |
|
Appropriately designed checklists may reduce errors of omission and improve patient outcomes |
|
The intubation team should consist of at least three healthcare providers, including two airway operators (one of whom should be experienced) |
|
Training requirements should be well-defined and include simulation-based training |
|
Patient preparation and optimization |
|
Screen critically ill adults requiring tracheal intubation for both anatomic and physiologic difficulty |
|
Hemodynamics should be optimized prior to tracheal intubation |
|
Point-of-care ultrasound aids the assessment and management of cardio-respiratory compromise |
|
Preoxygenation with non-invasive ventilation is preferred, and high flow nasal oxygen can be used to facilitate oxygen delivery during apnea |
|
Careful mask ventilation may be performed to minimize desaturation |
|
Sub-anesthetic doses of sedative hypnotics to facilitate pre-oxygenation while maintaining spontaneous ventilation (i.e., delayed sequence intubation) can be considered in patients who would otherwise be difficult to pre-oxygenate |
|
Performing the procedure |
|
Modified rapid sequence intubation should be considered |
|
Ketamine or etomidate are the preferred sedative hypnotic agents, and standard anesthetic induction doses of propofol should be avoided |
|
Video laryngoscopy should be available and routinely employed during the first tracheal intubation attempt |
|
A stylet or bougie should be routinely employed |
|
Post-intubation care |
|
Tracheal tube placement should be confirmed using waveform capnography with consistent rise in amplitude during exhalation, with decline during inspiration, over at least seven breaths |
|
Fluid responsiveness should be re-evaluated using dynamic indices before fluid administration in patients who develop hemodynamic instability |
|
Invasive vascular access should be established in patients who develop persistent hemodynamic instability |
|
Sedative hypnotic infusions guided by clinically assessed sedation depth should be used to reduce the risk of accidental awareness with recall in patients who received neuromuscular blocking agents |
It is also important to emphasize that dissensus and/or disagreement among experts was also identified in several areas, including: the definition of an experienced airway operator, the role and management of cricoid pressure, the optimal video laryngoscope design (e.g., conventional versus hyperangulated), and the importance of routinely reversing neuromuscular blocking agents after tracheal intubation. Apart from these domains, the need to further appraise interventions to prevent cardiovascular collapse—the most common physiologic complication associated with tracheal intubation in critically ill adults—emerged as an important area for future research as current evidence is markedly lacking to adequately inform our clinical practice. Work will also be needed to further bridge the implementation gap between identified best practices and the bedside, including identifying barriers to the universal availability and application of video laryngoscopy in this patient population, developing optimal approaches to the application of point-of-care ultrasound, PDA curriculum development, and adaptation to resource limited environments.
On behalf of SOCCA’s PDA Task Force, we would like to extend a token of thanks to all SOCCA members who made this work possible, including Task Force members and those who participated as experts in the consensus effort.