Healthcare worker risk of contracting COVID-19 after vaccination
We previously reviewed data related to the risk of healthcare workers contracting COVID-19 in December of 2020 (Interchange:31[3]). One study of front-line healthcare workers demonstrated a 4% positive COVID-19 testing rate compared to just 0.33% for the general population1. In a survey study of 105 anesthesiologists and intensivists at a New York City hospital, 58% reported a workplace exposure (mostly related to airway management), 26% of those reported COVID-19-like symptoms after that exposure, but only 12% of providers tested were found to be positive for antibodies 2. That was the same incidence of positive antibody testing for those reporting no exposure, and the authors concluded the COVID-19 infections were most likely community-acquired. A study looking at healthcare workers performing a high-risk procedure—intubation—showed that the risk of transmission, hospitalization, and/or self-quarantine was approximately 10%3.
Since our last update on this topic, there are now three options for SARS-CoV-2 vaccination in the U.S. During the initial roll out of vaccination programs, two mRNA-based vaccines were available, both showing high efficacy. The Pfizer-BioNTech trial had only 8 cases of COVID-19 out of 21,720 vaccinated participants (incidence of 0.04%) seven or more days after the second dose of vaccine 4. The Moderna trial had only 11 symptomatic confirmed COVID-19 cases out of 15,210 in the vaccine group, for an incidence of 0.07% 5. Despite these very encouraging results, in addition to the overall safety of the vaccine, COVID-19 vaccine hesitancy remains high, even among healthcare workers 6,7.
Despite that hesitancy, a large percentage of the healthcare workforce is now vaccinated against SARS-CoV-2, and studies are becoming available to help us assess the risk of developing asymptomatic and symptomatic infection after vaccination. All three studies described below used mRNA vaccines.
The University of Texas Southwestern Medical Center studied the effect of vaccination in their 23,234 healthcare workers. In the study time period, approximately 9,000 people were not vaccinated, 13,700 received one dose of an mRNA vaccine, and nearly 7,000 people received two doses 8. The incidence of infection (i.e., a positive SARS-CoV-2 PCR test) varied based on vaccination status: 2.6% in healthcare workers who had not yet received any vaccination, 1.8% after one dose, and 0.05% after two doses.
A study at the University of California, San Diego (UCSD) and the University of California, Los Angeles (UCLA) looked at a population of 36,659 healthcare workers who received the first dose of one of the mRNA vaccines 9. Of those, 28,184 had also received the second dose. Like the previously mentioned study, the incidence of COVID-19 infection varied by vaccination status. In the first two weeks following vaccination, about 2% of tested individuals resulted positive. In contrast, eight or more days after the second dose, only 0.17% of tests were positive. Of note, the absolute risk of a positive test in this group was 1.19% at UCSD and 0.97% at UCLA, higher than the risks reported in the trials for the mRNA vaccines. This may be explained by the low threshold these institutions had for testing symptomatic employees, and UCSD performed asymptomatic testing on a weekly basis. No testing of asymptomatic participants occurred in the Pfizer-BioNTech trial of the BNT162b2 mRNA vaccine.
Finally, a study at the Hadassah Hebrew University Medical Center in Jerusalem, Israel, looked at positive SARS-CoV-2 PCR rates in their healthcare workforce before and after vaccinations with the Pfizer-BioNTech mRNA vaccine. In the months before vaccination efforts ramped up, 10.3% of 6,680 health care workers tested positive [10]. Most were determined to be due to community exposures. Similar to the other studies, the rate of healthcare worker positive tests dropped dramatically after vaccine roll out. Two weeks after receiving the second dose, only 2 healthcare workers tested positive out of 4,793 people who had received both doses (incidence 0.04%).
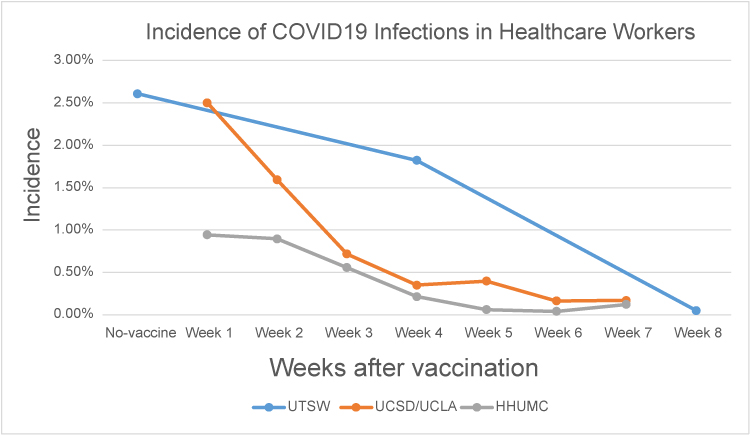
HHUMC, Hadassah Hebrew University Medical Center in Jerusalem; UTSW, The University of Texas Southwestern Medical Center; UCSD/UCLA, University of California San Diego/University of California Los Angeles. Data derived from 8-10
The data in healthcare workers clearly shows that vaccination dramatically reduces the incidence of a positive SARS-CoV-2 PCR test. These data correlate well with mRNA vaccine phase 3 trial data. As previously noted, the data are limited on the transmission risk during high-risk procedures like intubation, which in a pre-vaccine era were thought to be as high as 10% 3. Therefore, anesthesiologists and intensivists are likely to remain at relatively high risk of infection. As such, addressing any vaccine hesitancy in this high-risk group of providers should be a top priority.
References
- Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475-e483.
- Morcuende M, Guglielminotti J, Landau R. Anesthesiologists' and intensive care providers' exposure to COVID-19 infection in a new york city academic center: a prospective cohort study assessing symptoms and COVID-19 antibody testing. Anesth Analg. 2020;131(3):669-676.
- El-Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. 2020;75(11):1437-1447.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603-2615.
- Baden LR, El Sahly HM, Essink B, et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384(5):403-416.
- Kuter BJ, Browne S, Momplaisir FM, et al. Perspectives on the receipt of a COVID-19 vaccine: a survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39(12):1693-1700.
- Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel). 2021;9(2).
- Daniel W, Nivet M, Warner J, Podolsky DK. Early evidence of the effect of SARS-CoV-2 vaccine at one medical center. N Engl J Med. 2021. Available at: https://doi.org/10.1056/NEJMc2102153
- Keehner J, Horton LE, Pfeffer MA, et al. SARS-CoV-2 infection after vaccination in health care workers in California. N Engl J Med. 2021. Available at: https://doi.org/10.1056/NEJMc2101927
- Benenson S, Oster Y, Cohen MJ, Nir-Paz R. BNT162b2 mRNA COVID-19 vaccine effectiveness among health care workers. N Engl J Med. 2021. Available at: https://doi.org/10.1056/NEJMc2101951





































